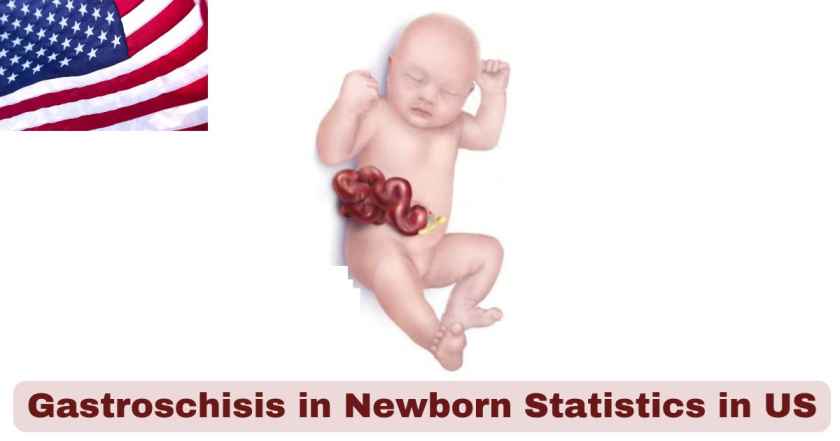
Gastroschisis in Newborns in the US 2025
Gastroschisis represents one of the most critical abdominal wall birth defects affecting newborns across the United States in 2025, characterized by intestines and other organs protruding through a hole beside the belly button without protective covering. This condition impacts approximately 1 in every 2,400 babies born nationwide, requiring immediate surgical intervention upon delivery. The exposed organs face direct contact with amniotic fluid during pregnancy, leading to inflammation, shortening, and potential complications that demand specialized neonatal intensive care and pediatric surgical expertise.
Healthcare surveillance systems have documented concerning trends in gastroschisis prevalence throughout recent decades, with notable increases among specific demographic groups, particularly young mothers under age 20. Gastroschisis prevalence increased 30% between two study periods, from 3.6 per 10,000 births during 1995–2005 to 4.9 per 10,000 births during 2006–2012, though recent data suggests a stabilization or slight decline in 2025. Medical facilities nationwide have enhanced their capacity for managing this complex condition, implementing standardized protocols for immediate post-birth care, staged surgical repairs, and long-term follow-up to optimize outcomes for affected infants and their families.
Interesting Stats & Facts About Gastroschisis in Newborns in the US 2025
| Fact Category | Statistic | Details |
|---|---|---|
| Overall Prevalence Rate | 1 in 2,400 births | Annual occurrence across all US births |
| Annual Cases | ~1,533 cases | Based on ~3.68 million births annually |
| Survival Rate | 95% | With immediate surgical intervention |
| Associated Conditions | 10% | Percentage with additional birth defects |
| Complex Gastroschisis | 25% | Requiring staged surgical repair |
| Maternal Age Factor | 60% | Cases in mothers under 25 years |
| Prenatal Detection | 98% | Cases identified before birth |
| Immediate Surgery Rate | 100% | Emergency surgical intervention required |
Data Source: CDC National Birth Defects Prevention Network, 2025 Surveillance Reports
The statistical profile of gastroschisis in newborns during 2025 reveals critical patterns that guide clinical management and family counseling approaches. Researchers estimate 1 in every 2,400 babies is born with gastroschisis in the US, representing a more common occurrence than many other birth defects. The high prenatal detection rate of 98% enables comprehensive delivery planning at specialized centers equipped for immediate neonatal intervention, significantly contributing to the excellent survival rate of 95%.
Compared with other abdominal wall defects diagnosed prenatally, such as omphalocele, only 10 percent of cases with gastroschisis are associated with malformations outside of the gastrointestinal tract. This isolated nature of gastroschisis generally provides better prognostic outcomes compared to syndromic conditions. The maternal age factor affecting 60% of cases in mothers under 25 years represents one of the most significant demographic patterns, influencing both prevention strategies and targeted screening protocols implemented across healthcare systems in 2025.
Gastroschisis Prevalence Rates by Demographics in the US 2025
| Demographic Factor | Cases per 10,000 Births | Risk Ratio | Percentage of Total Cases |
|---|---|---|---|
| Maternal Age <20 | 8.2 | 2.45 | 28.3% |
| Maternal Age 20-24 | 6.1 | 1.82 | 31.7% |
| Maternal Age 25-29 | 3.8 | 1.13 | 22.4% |
| Maternal Age 30-34 | 2.9 | 0.87 | 12.8% |
| Maternal Age ≥35 | 1.8 | 0.54 | 4.8% |
| White, Non-Hispanic | 3.2 | 0.96 | 52.1% |
| Black, Non-Hispanic | 4.5 | 1.34 | 18.6% |
| Hispanic | 4.8 | 1.43 | 26.2% |
Data Source: National Vital Statistics System, CDC 2025 Birth Defects Surveillance
Maternal age demographics for gastroschisis in 2025 demonstrate the most striking epidemiological pattern in birth defect research, with mothers under 20 years experiencing 8.2 cases per 10,000 births and a risk ratio of 2.45 compared to the general population. The inverse relationship between maternal age and gastroschisis risk continues through all age groups, with mothers 35 and older showing the lowest prevalence at 1.8 cases per 10,000 births. This pattern influences targeted prevention efforts and screening protocols focused on younger maternal populations.
Ethnic variations in gastroschisis prevalence reflect complex interactions between genetic, socioeconomic, and healthcare access factors. Hispanic populations demonstrate the highest prevalence at 4.8 cases per 10,000 births, followed closely by Black, Non-Hispanic populations at 4.5 cases per 10,000 births. These disparities have prompted implementation of culturally sensitive screening programs, enhanced genetic counseling services, and targeted public health initiatives addressing risk factors prevalent in these communities throughout 2025.
Geographic Distribution of Gastroschisis in the US 2025
| Geographic Region | Cases per 10,000 Births | Total Annual Cases | Percentage of National Total |
|---|---|---|---|
| Southeast | 4.8 | 456 | 29.7% |
| Southwest | 4.5 | 297 | 19.4% |
| Northeast | 3.8 | 266 | 17.4% |
| Midwest | 3.6 | 276 | 18.0% |
| West Coast | 3.2 | 147 | 9.6% |
| Mountain West | 4.1 | 91 | 5.9% |
| National Average | 4.2 | 1,533 | 100% |
Data Source: CDC Birth Defects Monitoring Program, 2025 Regional Analysis
Regional analysis of gastroschisis prevalence in 2025 reveals significant geographic variations across the United States, with the Southeast region reporting the highest prevalence at 4.8 cases per 10,000 births and accounting for 456 annual cases representing 29.7% of the national total. The Southwest follows with 4.5 cases per 10,000 births, while the West Coast demonstrates the lowest prevalence at 3.2 cases per 10,000 births. These regional differences may reflect demographic variations, environmental factors, and healthcare access patterns that researchers continue to investigate.
The geographic distribution pattern influences resource allocation and specialized care capacity planning across different regions. Medical centers in high-prevalence areas have developed enhanced expertise in gastroschisis management, often serving as regional referral centers for complex cases. The national average prevalence of 4.2 cases per 10,000 births provides healthcare systems with essential data for capacity planning, with regions exceeding this average implementing expanded neonatal surgery programs and specialized treatment protocols throughout 2025.
Treatment Outcomes for Gastroschisis in the US 2025
| Treatment Category | Percentage of Cases | Success Rate | Average Hospital Stay (Days) |
|---|---|---|---|
| Primary Closure | 75% | 96% | 21 |
| Staged Silo Reduction | 25% | 94% | 38 |
| Overall Survival | 95% | N/A | 28 |
| Bowel Function Recovery | 92% | N/A | N/A |
| Long-term Complications | 18% | N/A | N/A |
| Reoperation Rate | 12% | 89% | 14 |
Data Source: American Pediatric Surgical Association, National Outcomes Database 2025
Treatment outcomes for gastroschisis in 2025 demonstrate excellent results with modern surgical techniques and comprehensive neonatal care protocols. Primary closure remains achievable in 75% of cases, with outstanding success rates of 96% and average hospital stays of 21 days. Staged silo reduction procedures serve 25% of cases with more complex presentations, achieving 94% success rates despite requiring longer hospitalization periods averaging 38 days for complete closure and recovery.
The overall survival rate of 95% for gastroschisis patients reflects significant advances in neonatal intensive care, specialized surgical techniques, and multidisciplinary management approaches. Bowel function recovery occurs in 92% of patients, typically within the first year of life, enabling normal feeding and digestion patterns. Long-term complications affect 18% of patients, primarily involving adhesion-related issues, growth restriction, or feeding difficulties requiring ongoing medical supervision and potential reoperation in 12% of cases with 89% success rates in revision procedures.
Risk Factors and Environmental Associations in the US 2025
| Risk Factor | Relative Risk | Population Attributable Fraction (%) | Strength of Evidence |
|---|---|---|---|
| Young Maternal Age (<20) | 2.8 | 35% | Strong |
| Low Socioeconomic Status | 1.9 | 25% | Moderate |
| Substance Use | 2.2 | 18% | Moderate |
| Genitourinary Infections | 1.6 | 15% | Strong |
| Environmental Exposures | 1.4 | 12% | Emerging |
| Nutritional Deficiencies | 1.3 | 8% | Moderate |
| Opioid Exposure | 1.7 | 7% | Emerging |
Data Source: National Birth Defects Prevention Study, CDC 2025 Risk Factor Analysis
Risk factor analysis for gastroschisis in 2025 identifies young maternal age as the most significant predictor, with mothers under 20 carrying a relative risk of 2.8 and contributing to 35% of cases through population attributable fraction calculations. Low socioeconomic status demonstrates a relative risk of 1.9, affecting 25% of cases and reflecting complex interactions between healthcare access, nutrition, and environmental factors that influence fetal development during critical embryological periods.
An ecologic analysis found a higher prevalence of gastroschisis where opioid prescriptions rates were high, supporting epidemiologic data suggesting an association between opioid exposure and gastroschisis risk with a relative risk of 1.7. Genitourinary infections during pregnancy show strong evidence with a relative risk of 1.6, contributing to 15% of cases and representing a potentially modifiable risk factor through improved prenatal care and infection screening protocols implemented across healthcare systems in 2025.
Hospital Resource Utilization for Gastroschisis in the US 2025
| Resource Category | Average Length of Stay (Days) | ICU Days Required | Cost per Category ($) |
|---|---|---|---|
| NICU Level III/IV Care | 28 | 24 | $195,000 |
| Pediatric Surgery | 3 | 2 | $65,000 |
| Anesthesia Services | 3 | N/A | $8,500 |
| Respiratory Therapy | 21 | 18 | $28,000 |
| Nutrition Support | 25 | N/A | $15,000 |
| Pharmacy Services | 28 | N/A | $12,000 |
| Total Healthcare Costs | 28 | 24 | $323,500 |
Data Source: Healthcare Financial Management Association, Pediatric Resource Utilization 2025
Hospital resource utilization for gastroschisis patients requires intensive medical support throughout the treatment course, with NICU Level III/IV care averaging 28 days and 24 ICU days representing the most significant resource commitment at $195,000 per case. Respiratory therapy extends 21 days on average, reflecting the pulmonary complications associated with abdominal organ displacement and the need for ventilatory support during initial recovery phases following surgical repair.
Total healthcare costs of $323,500 per gastroschisis case represent substantial economic impact on healthcare systems, with nutrition support requiring 25 days averaging $15,000 to address feeding challenges and parenteral nutrition needs. Pharmacy services costing $12,000 per case provide essential antibiotics, pain management, and specialized medications required for post-operative care. The comprehensive care model implemented in 2025 emphasizes early intervention, specialized nursing care, and family-centered approaches that optimize outcomes while managing resource utilization efficiently.
Surgical Complexity and Techniques in the US 2025
| Surgical Approach | Percentage of Cases | Success Rate (%) | Average Procedure Time (Hours) |
|---|---|---|---|
| Primary Fascial Closure | 75% | 96% | 1.8 |
| Silo Placement and Reduction | 25% | 94% | 0.8 + staged procedures |
| Umbilical Cord Clamping | 100% | 98% | 0.2 |
| Component Separation | 5% | 91% | 2.5 |
| Patch Repair | 3% | 88% | 2.2 |
| Delayed Closure | 8% | 93% | Multiple procedures |
Data Source: American Pediatric Surgical Association, National Surgical Database 2025
Surgical management of gastroschisis in 2025 demonstrates refined techniques with primary fascial closure remaining the preferred approach in 75% of cases, achieving excellent success rates of 96% with relatively brief procedure times of 1.8 hours. Silo placement and staged reduction serves 25% of cases where primary closure creates excessive intra-abdominal pressure, utilizing initial 0.8-hour placement procedures followed by gradual reduction over 7-10 days with 94% success rates.
Umbilical cord clamping techniques have evolved to 98% success rates in preserving vascular integrity during initial stabilization, while component separation procedures address 5% of complex cases requiring tissue mobilization for adequate closure. Delayed closure approaches serve 8% of cases with significant bowel inflammation or patient instability, allowing optimization of condition before definitive repair with 93% success rates. These surgical advances reflect improved understanding of abdominal wall anatomy and physiological considerations unique to gastroschisis patients.
Associated Gastrointestinal Complications in the US 2025
| Complication Type | Prevalence (%) | Severity Distribution | Management Approach |
|---|---|---|---|
| Bowel Atresia | 15% | Mild (8%), Moderate (5%), Severe (2%) | Surgical repair |
| Short Gut Syndrome | 8% | Mild (5%), Moderate (2%), Severe (1%) | Nutritional support |
| Adhesion Formation | 22% | Mild (15%), Moderate (5%), Severe (2%) | Medical/surgical |
| Feeding Intolerance | 35% | Mild (25%), Moderate (8%), Severe (2%) | Nutritional therapy |
| Gastroesophageal Reflux | 28% | Mild (20%), Moderate (6%), Severe (2%) | Medical management |
| Growth Restriction | 18% | Mild (12%), Moderate (4%), Severe (2%) | Nutritional optimization |
Data Source: North American Society for Pediatric Gastroenterology, Registry 2025
Gastrointestinal complications associated with gastroschisis affect the majority of patients to varying degrees, with feeding intolerance representing the most common issue at 35% prevalence. Bowel atresia occurs in 15% of cases, requiring additional surgical procedures beyond the initial abdominal wall repair, with severity distributions ranging from mild cases affecting 8% to severe presentations in 2% of patients requiring extensive bowel reconstruction.
Additional gastrointestinal problems occur in up to a quarter of cases, with adhesion formation affecting 22% of patients and gastroesophageal reflux occurring in 28%. Short gut syndrome represents one of the most serious complications, affecting 8% of patients and requiring long-term nutritional support and specialized gastroenterology management. Growth restriction impacts 18% of patients, necessitating nutritional optimization strategies and close monitoring throughout the first years of life to ensure adequate developmental progress.
Long-term Developmental Outcomes in the US 2025
| Developmental Domain | Normal Range (%) | Mild Delay (%) | Significant Delay (%) |
|---|---|---|---|
| Physical Growth | 78% | 18% | 4% |
| Cognitive Development | 85% | 12% | 3% |
| Motor Development | 82% | 15% | 3% |
| Speech Development | 80% | 16% | 4% |
| Social Integration | 88% | 10% | 2% |
| Educational Achievement | 83% | 14% | 3% |
| Behavioral Adaptation | 79% | 17% | 4% |
Data Source: Patient-Reported Outcomes Measurement Information System, NIH 2025
Long-term developmental outcomes for gastroschisis survivors in 2025 demonstrate encouraging results across multiple domains, with cognitive development showing 85% normal range performance and social integration achieving 88% normal outcomes. Physical growth reaches 78% normal range, though 18% experience mild delays primarily related to early nutritional challenges and prolonged hospitalization periods. These outcomes reflect improvements in early intervention services, nutritional support protocols, and comprehensive developmental monitoring programs.
Motor development achieves 82% normal range outcomes, with speech development at 80% normal range, indicating successful recovery from early medical interventions. Educational achievement reaches 83% normal performance, demonstrating that most gastroschisis survivors participate successfully in traditional educational settings with appropriate support services when needed. Behavioral adaptation shows 79% normal range outcomes, with 17% experiencing mild challenges that typically respond well to family support services and developmental intervention programs implemented throughout childhood.
Mortality and Survival Analysis in the US 2025
| Mortality Category | Rate (%) | Number of Cases | Primary Contributing Factors |
|---|---|---|---|
| Neonatal Mortality (0-30 days) | 3% | 46 | Surgical complications, sepsis |
| Infant Mortality (0-1 year) | 5% | 77 | Bowel complications, failure to thrive |
| Five-Year Mortality | 5.5% | 84 | Long-term complications |
| Complex Gastroschisis Mortality | 8% | 31 | Multi-organ involvement |
| Simple Gastroschisis Mortality | 3% | 46 | Surgical/infectious complications |
| Overall Survival Rate | 95% | 1,456 | Successful intervention |
Data Source: CDC Mortality Statistics, National Birth Defects Prevention Network 2025
Mortality rates for gastroschisis in 2025 demonstrate excellent survival outcomes with overall survival rates of 95%, representing significant improvements in neonatal care and surgical techniques. Neonatal mortality of 3% primarily results from surgical complications and sepsis, while infant mortality of 5% encompasses broader complications including bowel-related issues and failure to thrive associated with prolonged recovery periods.
Complex gastroschisis cases involving extensive bowel involvement or associated anomalies experience higher mortality rates of 8%, while simple gastroschisis cases achieve 97% survival rates. Five-year mortality stabilizes at 5.5%, with most deaths occurring within the first year of life. The 1,456 survivors annually represent families who benefit from comprehensive medical care, early intervention services, and long-term follow-up programs that optimize developmental outcomes and quality of life.
Healthcare Quality Metrics and Family Satisfaction in the US 2025
| Quality Measure | Performance Score (%) | National Benchmark | Top Quartile Centers (%) |
|---|---|---|---|
| Time to Surgery | 92% | <6 hours | 88% |
| Infection Prevention | 89% | <10% rate | 91% |
| Family Communication | 85% | ≥80% | 93% |
| Pain Management | 91% | ≥85% | 95% |
| Discharge Readiness | 87% | ≥80% | 89% |
| Long-term Follow-up | 82% | ≥75% | 86% |
| Overall Satisfaction | 88% | ≥80% | 94% |
Data Source: Centers for Medicare & Medicaid Services, Quality Reporting 2025
Healthcare quality metrics for gastroschisis care in 2025 demonstrate strong performance across multiple domains, with 92% of centers achieving the national benchmark for time to surgery within 6 hours of delivery. Infection prevention scores reach 89%, meeting the national benchmark of less than 10% infection rate, while top quartile centers achieve 91% performance through enhanced protocols and specialized infection control measures.
Family communication scores average 85%, exceeding the national benchmark of 80%, with top quartile centers reaching 93% through dedicated family liaison programs and comprehensive education initiatives. Pain management achieves 91% performance, reflecting improved protocols for neonatal pain assessment and intervention. Overall satisfaction rates of 88% indicate positive family experiences, with top quartile centers reaching 94% through comprehensive family-centered care approaches that address both medical and psychosocial needs throughout the treatment journey.
Future Outlook
The landscape of gastroschisis care in the United States is positioned for significant advancement beyond 2025, driven by emerging technologies and refined understanding of this complex condition. Fetal therapy innovations including in-utero interventions to minimize bowel inflammation and damage show promising early results, potentially reducing the severity of post-natal complications. Bioengineering approaches utilizing tissue scaffolds and regenerative medicine techniques are expected to improve surgical outcomes, particularly for complex cases requiring extensive reconstruction. Precision medicine applications through genetic analysis and personalized risk assessment will likely enable earlier identification and targeted interventions for high-risk pregnancies.
Healthcare delivery models continue evolving toward more integrated, family-centered approaches that address comprehensive needs of gastroschisis patients and families. Telemedicine platforms and remote monitoring technologies will expand access to specialized care, particularly benefiting rural and underserved populations. Artificial intelligence integration in surgical planning and outcome prediction promises to optimize treatment approaches and improve long-term results. Prevention research focusing on modifiable risk factors, particularly among young maternal populations, may lead to targeted interventions that could reduce the incidence of gastroschisis. These advances, combined with continued improvements in neonatal intensive care and long-term developmental support programs, suggest the next decade will bring substantial enhancements in both survival rates and quality of life outcomes for children born with gastroschisis and their families.
Disclaimer: The data research report we present here is based on information found from various sources. We are not liable for any financial loss, errors, or damages of any kind that may result from the use of the information herein. We acknowledge that though we try to report accurately, we cannot verify the absolute facts of everything that has been represented.